Decontamination is essential in dental clinics to ensure the safety of both patients and dental healthcare providers. Through the use of effective and reliable decontamination equipment and practices, you can minimise the risk of cross-contamination and the transmission of infectious diseases between patients and dental staff.
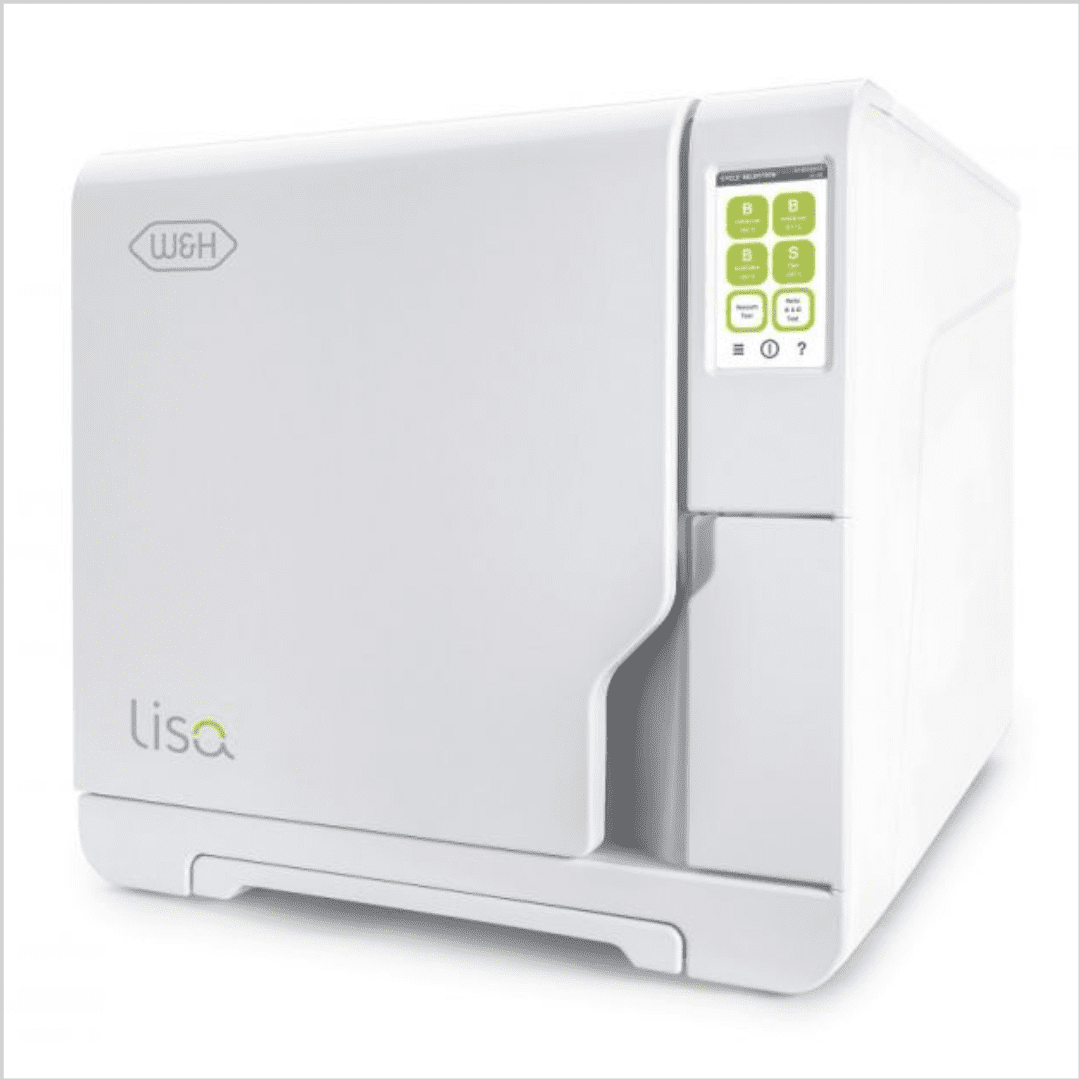
Class N, S and B autoclaves
Class N-Type autoclaves use steam from a boiler or generator to create downward displacement, which pushes air out of the chamber. Class N-Type autoclaves do not guarantee 100% air removal. The letter “N” stands for “naked solid products” therefore, these autoclaves cannot be used to sterilise textiles, porous loads, hollow items or even products in pouches, as the cycles do not have the right characteristics to pass specific physical tests.
Class S-Type autoclaves allow for the sterilisation of single-packed, multilayer packed and larger instruments, which you cannot sterilise in Class N-Type autoclaves. Class S-Type autoclaves have a vacuum pump, making it possible to remove the air from the chamber altogether before starting the sterilisation process.
Class B-Type autoclaves comply with the strictest sterilisation standards and regulations and use a pre-vacuum cycle to remove air from the sterilisation chamber to help ensure efficient steam penetration. They can sterilise a wide range of loads, including solid instruments, hollow instruments, and porous items, and are highly effective in killing microorganisms.
Legislation
Dental clinics are subject to various regulations and guidelines that outline infection control requirements. Adhering to these regulations is crucial for maintaining the clinic’s license, reputation, and ensuring patient safety:
HTM 01-05 is a set of guidelines published by the Department of Health and Social Care in the UK. It provides comprehensive guidance on infection prevention and control in dental practices. HTM 01-05 outlines the specific requirements for the decontamination and sterilisation of dental instruments and equipment, including the use of autoclaves. It covers topics such as equipment selection, maintenance, validation, and monitoring of autoclaves.
- Care Quality Commission (CQC) regulations: The CQC is the independent regulator of healthcare services in England. Dental practices are inspected by the CQC to ensure compliance with regulations, including those related to infection prevention and control. While the Care Quality Commission (CQC) does not explicitly state that B-type autoclaves are required, compliance with the HTM 01-05 guidelines is considered essential for dental practices to meet the CQC’s infection prevention and control standards. Therefore, dental practices are expected to follow the recommended best practices outlined in HTM 01-05, which include using Class B-Type autoclaves for hollow instrument sterilisation.
How many autoclaves should my practice have?
The specific number of autoclaves required for a dental practice under the Care Quality Commission (CQC) regulations in the UK may vary depending on factors such as the size of the practice, the volume of patient procedures, and the availability of alternative sterilisation methods. The CQC does not provide a specific requirement for the number of autoclaves a dental practice should have. However, dental practices are expected to have sufficient autoclaves to meet their sterilisation needs and ensure compliance with infection prevention and control guidelines.
When determining the number of autoclaves for your dental practice, consider the following factors:
Workflow and patient load: Evaluate the number of patient procedures conducted in your practice and the associated instrument sterilisation requirements. This will help you estimate the capacity needed to handle the workload efficiently.
Instrument turnover time: Consider the time required to clean, disinfect, package, and sterilise instruments. If your practice has a high instrument turnover rate, you may need multiple autoclaves to keep up with the demand and maintain smooth workflow.
Redundancy and maintenance: It’s important to have contingency plans in case of equipment breakdown or maintenance. Having additional autoclaves or alternative sterilisation methods can help ensure uninterrupted sterilisation processes.
Compliance with guidelines: Ensure that your dental practice can meet the guidelines outlined in HTM 01-05 and other relevant guidance related to instrument decontamination and sterilisation. This includes having adequate equipment to fulfil the necessary sterilisation requirements.
It is recommended to consult with equipment manufacturers, infection control experts, or dental professional organisations for guidance specific to your practice’s needs. They can provide valuable insights on the optimal number of autoclaves required based on industry best practices, regulatory requirements, and the specific circumstances of your dental practice.
A clean and hygienic environment also promotes patient confidence and trust. When patients see that proper decontamination practices are followed, they are more likely to feel comfortable and secure during their dental visits.